The Science of Blood Sugar Regulation: How Your Body Balances Energy
- Dr. Sean

- Sep 26, 2025
- 4 min read
Disclaimer: This article is provided for educational purposes only and is not intended as medical advice. Please consult a healthcare professional for personal guidance.

Introduction: Why Blood Sugar Matters
Every cell in the human body depends on energy, and glucose—commonly referred to as “blood sugar”—is the fuel of choice. From powering the brain’s billions of neurons to supporting muscles during activity, glucose provides the energy required for life.
Yet glucose must be maintained within a narrow range. Too high, and it damages blood vessels and organs over time. Too low, and essential tissues such as the brain can no longer function properly. The balance of blood sugar, also known as glucose homeostasis, is therefore one of the most fundamental processes of human physiology.
In this article, we’ll explore how the body regulates blood sugar, what happens when regulation fails, and practical steps that can help keep glucose levels steady.
What Is Blood Sugar?
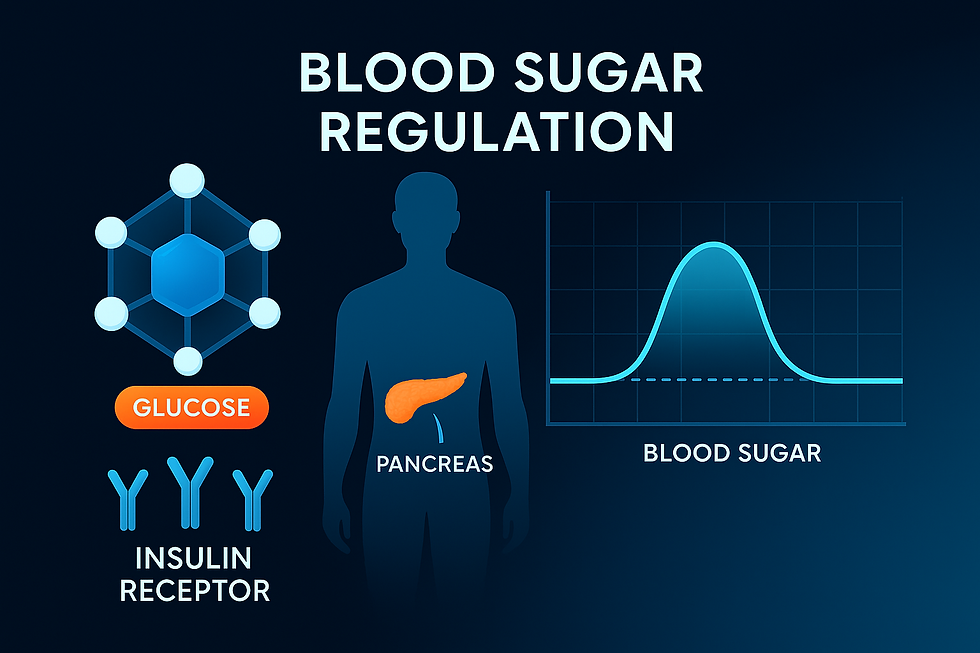
Blood sugar refers to the concentration of glucose circulating in the bloodstream, measured in milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L). In healthy individuals:
Fasting glucose typically falls between 70–99 mg/dL (3.9–5.5 mmol/L).
Post-meal glucose usually stays below 140 mg/dL (7.8 mmol/L) two hours after eating.
These values may vary slightly by clinical guidelines, but the principle is universal: blood sugar must stay within a safe and relatively stable range.
The Control System: Hormones and Organs
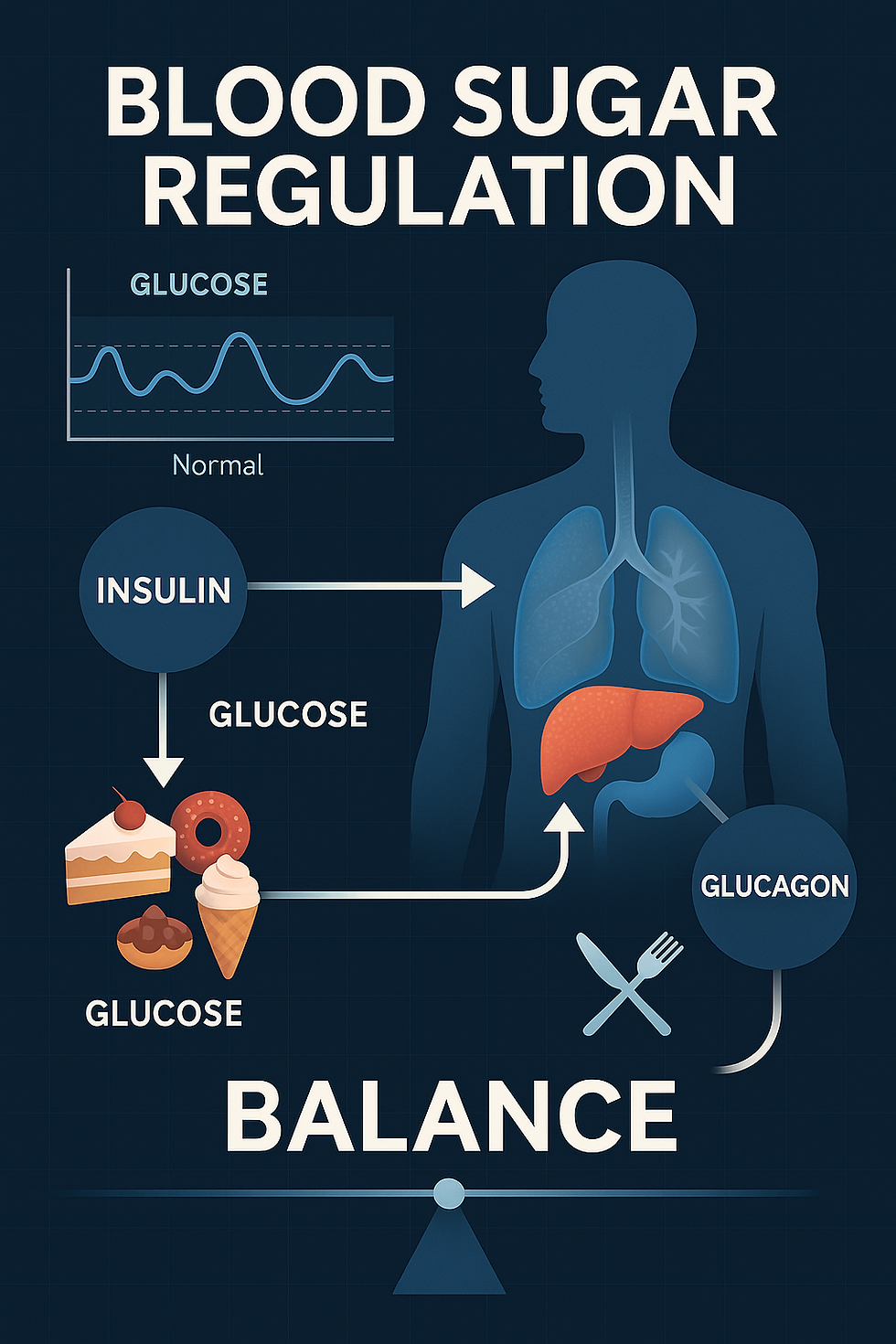
Blood sugar regulation works like a thermostat, automatically adjusting to keep levels stable. Several key hormones and organs are involved:
Insulin – Secreted by beta cells in the pancreas. When blood sugar rises after a meal, insulin signals cells (especially muscle, fat, and liver) to absorb glucose for energy or storage.
Glucagon – Produced by alpha cells in the pancreas. When blood sugar drops too low, glucagon triggers the liver to release stored glucose back into the blood.
Adrenaline (epinephrine) and cortisol – Stress hormones that prepare the body for “fight or flight.” They stimulate glucose release during stress or fasting.
The liver – Acts as the body’s glucose reservoir, storing glucose as glycogen and releasing it when needed.
The muscles – Consume glucose during activity; training increases their ability to use glucose efficiently.
This finely tuned system ensures that the brain—an organ that consumes around 20% of the body’s glucose—always has a steady energy supply.
What Happens When Regulation Fails?
High Blood Sugar (Hyperglycemia)
Chronic elevation of blood glucose, often due to insulin resistance, is a hallmark of type 2 diabetes. Over time, high blood sugar damages blood vessels, nerves, kidneys, eyes, and the cardiovascular system.
Low Blood Sugar (Hypoglycemia)
Too little glucose can cause dizziness, fatigue, sweating, and confusion. Severe hypoglycemia can be life-threatening because the brain relies almost entirely on glucose.
Both extremes highlight why balance is critical.
Everyday Strategies for Healthy Blood Sugar
Scientific research consistently shows that lifestyle factors have a profound effect on glucose regulation. Here are key strategies:
1. Eat Balanced, Low-GI Meals
Prioritize whole foods: Whole grains, legumes, vegetables, and lean proteins digest more slowly, leading to steadier glucose release.
Limit refined sugars and processed carbohydrates: These spike blood sugar quickly and can strain insulin response.
Pair carbs with protein and fat: This slows digestion and smooths out glucose fluctuations.
2. Exercise Regularly
Physical activity improves insulin sensitivity, meaning cells respond more effectively to insulin’s signal. Both aerobic exercise (like brisk walking or cycling) and strength training (like weightlifting) contribute to glucose control.
3. Manage Weight
Excess body fat, particularly visceral fat around the abdomen, increases insulin resistance. Maintaining a healthy weight significantly lowers the risk of type 2 diabetes.
4. Sleep and Stress Management
Poor sleep and chronic stress increase cortisol levels, which in turn elevate blood sugar. Prioritizing 7–8 hours of sleep and practicing stress-reduction techniques—such as meditation, yoga, or deep breathing—support glucose stability.
5. Monitor and Stay Informed
For people with higher risk, such as those with family history of diabetes, regular blood sugar checks are important. Tools like continuous glucose monitors (CGMs) are becoming more accessible, offering real-time feedback on how food and lifestyle impact blood sugar.
The Role of Nutrition Beyond Calories
In addition to macronutrients, research suggests that certain nutrients and bioactive compounds may play supportive roles in blood sugar regulation:
Dietary fiber (especially soluble fiber) slows glucose absorption, reducing spikes.
Magnesium and chromium are minerals linked to improved insulin sensitivity.
Plant extracts such as bitter melon, cinnamon polyphenols, and berberine have been studied for potential glucose-lowering effects.
It is important to emphasize that these are supportive, not replacements for medical treatment. A balanced diet and professional care remain the foundation.
Blood Sugar and Long-Term Health
Maintaining stable blood sugar doesn’t just prevent diabetes—it influences nearly every aspect of health:
Cardiovascular health: High blood sugar accelerates arterial damage.
Cognitive function: Glucose fluctuations are associated with brain fog and, in the long term, may influence cognitive decline.
Energy and mood: Stable glucose supports steady energy levels and fewer mood swings.
Healthy aging: Blood sugar balance is a cornerstone of metabolic health, directly linked to longevity.
Practical Tips for Daily Life
Start your day with a protein-rich breakfast rather than sugary cereals.
Choose water or unsweetened tea over sweetened drinks.
Take a 10–15 minute walk after meals to help muscles absorb glucose.
Prepare healthy snacks (nuts, yogurt, vegetables with hummus) to avoid high-sugar convenience foods.
Focus on consistency: small, sustainable habits matter more than perfection.
Conclusion: Balance Is the Key
Blood sugar regulation is one of the body’s most elegant balancing acts, keeping energy flowing while protecting vital organs. With the right lifestyle choices—balanced meals, regular activity, good sleep, and mindful stress management—most people can support this natural system and enjoy better health for years to come.
At Aset Nutrition, we are committed to advancing knowledge in nutrition and health. By understanding how blood sugar works and making science-based choices, individuals can take proactive steps toward long-term well-being.
Disclaimer
This content is for educational purposes only and is not a substitute for medical advice. Please consult a qualified healthcare professional for personal guidance.












